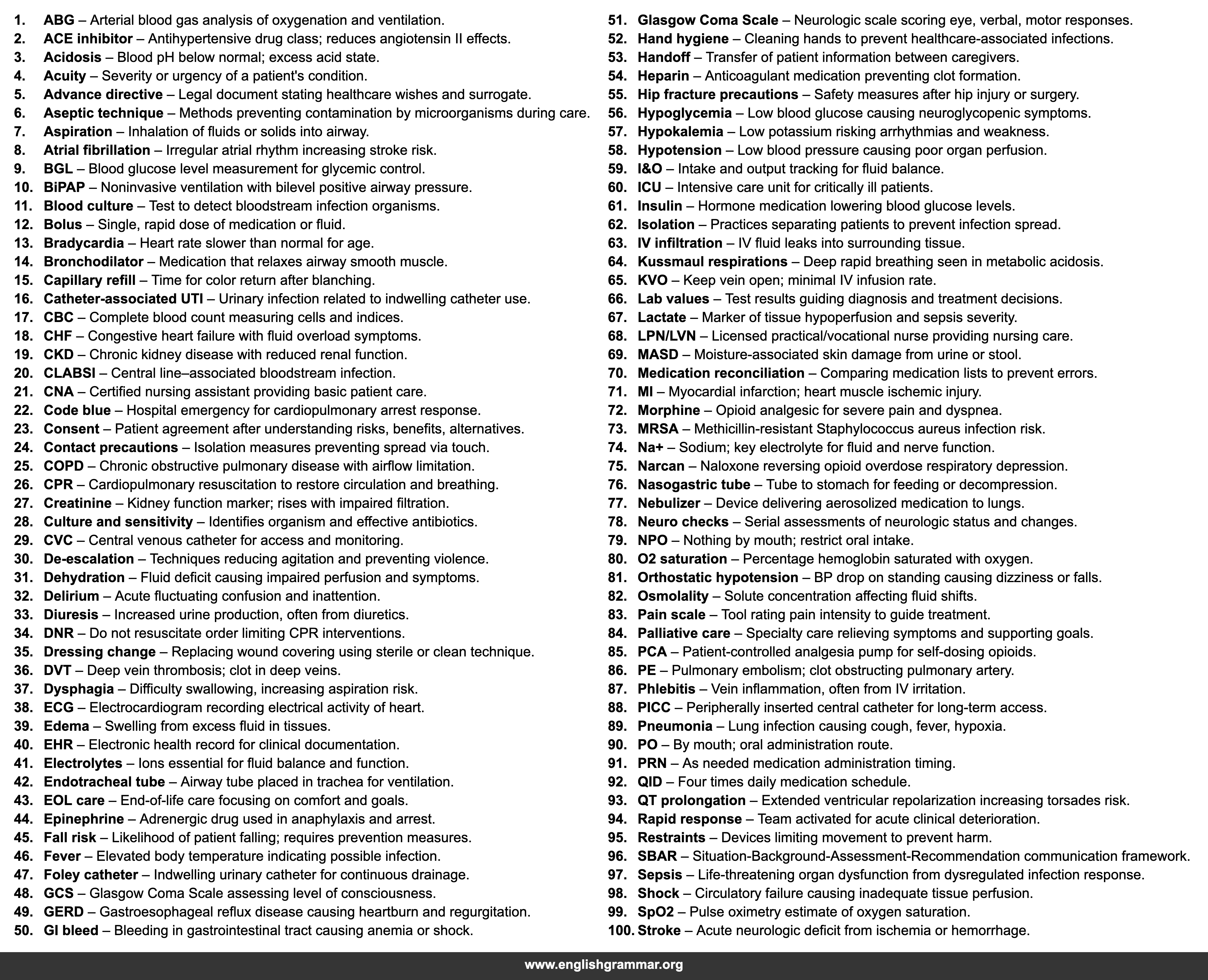
| No. | Term | Definition |
|---|---|---|
| 1. | ABG | Arterial blood gas analysis of oxygenation and ventilation. |
| 2. | ACE inhibitor | Antihypertensive drug class; reduces angiotensin II effects. |
| 3. | Acidosis | Blood pH below normal; excess acid state. |
| 4. | Acuity | Severity or urgency of a patient’s condition. |
| 5. | Advance directive | Legal document stating healthcare wishes and surrogate. |
| 6. | Aseptic technique | Methods preventing contamination by microorganisms during care. |
| 7. | Aspiration | Inhalation of fluids or solids into airway. |
| 8. | Atrial fibrillation | Irregular atrial rhythm increasing stroke risk. |
| 9. | BGL | Blood glucose level measurement for glycemic control. |
| 10. | BiPAP | Noninvasive ventilation with bilevel positive airway pressure. |
| 11. | Blood culture | Test to detect bloodstream infection organisms. |
| 12. | Bolus | Single, rapid dose of medication or fluid. |
| 13. | Bradycardia | Heart rate slower than normal for age. |
| 14. | Bronchodilator | Medication that relaxes airway smooth muscle. |
| 15. | Capillary refill | Time for color return after blanching. |
| 16. | Catheter-associated UTI | Urinary infection related to indwelling catheter use. |
| 17. | CBC | Complete blood count measuring cells and indices. |
| 18. | CHF | Congestive heart failure with fluid overload symptoms. |
| 19. | CKD | Chronic kidney disease with reduced renal function. |
| 20. | CLABSI | Central line–associated bloodstream infection. |
| 21. | CNA | Certified nursing assistant providing basic patient care. |
| 22. | Code blue | Hospital emergency for cardiopulmonary arrest response. |
| 23. | Consent | Patient agreement after understanding risks, benefits, alternatives. |
| 24. | Contact precautions | Isolation measures preventing spread via touch. |
| 25. | COPD | Chronic obstructive pulmonary disease with airflow limitation. |
| 26. | CPR | Cardiopulmonary resuscitation to restore circulation and breathing. |
| 27. | Creatinine | Kidney function marker; rises with impaired filtration. |
| 28. | Culture and sensitivity | Identifies organism and effective antibiotics. |
| 29. | CVC | Central venous catheter for access and monitoring. |
| 30. | De-escalation | Techniques reducing agitation and preventing violence. |
| 31. | Dehydration | Fluid deficit causing impaired perfusion and symptoms. |
| 32. | Delirium | Acute fluctuating confusion and inattention. |
| 33. | Diuresis | Increased urine production, often from diuretics. |
| 34. | DNR | Do not resuscitate order limiting CPR interventions. |
| 35. | Dressing change | Replacing wound covering using sterile or clean technique. |
| 36. | DVT | Deep vein thrombosis; clot in deep veins. |
| 37. | Dysphagia | Difficulty swallowing, increasing aspiration risk. |
| 38. | ECG | Electrocardiogram recording electrical activity of heart. |
| 39. | Edema | Swelling from excess fluid in tissues. |
| 40. | EHR | Electronic health record for clinical documentation. |
| 41. | Electrolytes | Ions essential for fluid balance and function. |
| 42. | Endotracheal tube | Airway tube placed in trachea for ventilation. |
| 43. | EOL care | End-of-life care focusing on comfort and goals. |
| 44. | Epinephrine | Adrenergic drug used in anaphylaxis and arrest. |
| 45. | Fall risk | Likelihood of patient falling; requires prevention measures. |
| 46. | Fever | Elevated body temperature indicating possible infection. |
| 47. | Foley catheter | Indwelling urinary catheter for continuous drainage. |
| 48. | GCS | Glasgow Coma Scale assessing level of consciousness. |
| 49. | GERD | Gastroesophageal reflux disease causing heartburn and regurgitation. |
| 50. | GI bleed | Bleeding in gastrointestinal tract causing anemia or shock. |
| 51. | Glasgow Coma Scale | Neurologic scale scoring eye, verbal, motor responses. |
| 52. | Hand hygiene | Cleaning hands to prevent healthcare-associated infections. |
| 53. | Handoff | Transfer of patient information between caregivers. |
| 54. | Heparin | Anticoagulant medication preventing clot formation. |
| 55. | Hip fracture precautions | Safety measures after hip injury or surgery. |
| 56. | Hypoglycemia | Low blood glucose causing neuroglycopenic symptoms. |
| 57. | Hypokalemia | Low potassium risking arrhythmias and weakness. |
| 58. | Hypotension | Low blood pressure causing poor organ perfusion. |
| 59. | I&O | Intake and output tracking for fluid balance. |
| 60. | ICU | Intensive care unit for critically ill patients. |
| 61. | Insulin | Hormone medication lowering blood glucose levels. |
| 62. | Isolation | Practices separating patients to prevent infection spread. |
| 63. | IV infiltration | IV fluid leaks into surrounding tissue. |
| 64. | Kussmaul respirations | Deep rapid breathing seen in metabolic acidosis. |
| 65. | KVO | Keep vein open; minimal IV infusion rate. |
| 66. | Lab values | Test results guiding diagnosis and treatment decisions. |
| 67. | Lactate | Marker of tissue hypoperfusion and sepsis severity. |
| 68. | LPN/LVN | Licensed practical/vocational nurse providing nursing care. |
| 69. | MASD | Moisture-associated skin damage from urine or stool. |
| 70. | Medication reconciliation | Comparing medication lists to prevent errors. |
| 71. | MI | Myocardial infarction; heart muscle ischemic injury. |
| 72. | Morphine | Opioid analgesic for severe pain and dyspnea. |
| 73. | MRSA | Methicillin-resistant Staphylococcus aureus infection risk. |
| 74. | Na+ | Sodium; key electrolyte for fluid and nerve function. |
| 75. | Narcan | Naloxone reversing opioid overdose respiratory depression. |
| 76. | Nasogastric tube | Tube to stomach for feeding or decompression. |
| 77. | Nebulizer | Device delivering aerosolized medication to lungs. |
| 78. | Neuro checks | Serial assessments of neurologic status and changes. |
| 79. | NPO | Nothing by mouth; restrict oral intake. |
| 80. | O2 saturation | Percentage hemoglobin saturated with oxygen. |
| 81. | Orthostatic hypotension | BP drop on standing causing dizziness or falls. |
| 82. | Osmolality | Solute concentration affecting fluid shifts. |
| 83. | Pain scale | Tool rating pain intensity to guide treatment. |
| 84. | Palliative care | Specialty care relieving symptoms and supporting goals. |
| 85. | PCA | Patient-controlled analgesia pump for self-dosing opioids. |
| 86. | PE | Pulmonary embolism; clot obstructing pulmonary artery. |
| 87. | Phlebitis | Vein inflammation, often from IV irritation. |
| 88. | PICC | Peripherally inserted central catheter for long-term access. |
| 89. | Pneumonia | Lung infection causing cough, fever, hypoxia. |
| 90. | PO | By mouth; oral administration route. |
| 91. | PRN | As needed medication administration timing. |
| 92. | QID | Four times daily medication schedule. |
| 93. | QT prolongation | Extended ventricular repolarization increasing torsades risk. |
| 94. | Rapid response | Team activated for acute clinical deterioration. |
| 95. | Restraints | Devices limiting movement to prevent harm. |
| 96. | SBAR | Situation-Background-Assessment-Recommendation communication framework. |
| 97. | Sepsis | Life-threatening organ dysfunction from dysregulated infection response. |
| 98. | Shock | Circulatory failure causing inadequate tissue perfusion. |
| 99. | SpO2 | Pulse oximetry estimate of oxygen saturation. |
| 100. | Stroke | Acute neurologic deficit from ischemia or hemorrhage. |